Utilization management is not an area of healthcare that most clinical nurses are particularly familiar with. Utilization management nurses do, however, play an important role in the behind-the-scenes clinical care of patients.
Utilization management nurses ensure that the care that has been provided or is going to be provided is necessary and the best use of resources.
So you can learn more about utilization management nurses, we’re going to cover the following topics:
- Where Do Utilization Management Nurses Work?
- How Do Utilization Management Nurses Help Patients?
- What Jobs Are Available as a Utilization Management Nurse?
- Job Outlook for Utilization Management Nurses
- What Is Working as a Utilization Management Nurse Like?
- How to Become a Utilization Management Nurse
Where Do Utilization Management Nurses Work?
Utilization management nurses often work for healthcare insurance companies, reviewing care that was provided and the claims that providers submit. They also work directly in hospitals to help improve efficiency.
Utilization management nurses working in insurance will often play an important role in determining if claims should be approved, reviewing appeals to claims, and participating in the prior authorization process.
While utilization management nurses may often work in healthcare insurance, this role is also important in hospitals and other care facilities.
Utilization management reviews help hospitals to ensure that staff and resources are allocated and used efficiently in the hospital, reducing unnecessary expenditures and cutting waste while ensuring that areas that require resources have the resources they need to function correctly.
Recommend readings:
How Do Utilization Management Nurses Help Patients?
Clinical nurses who are considering a career change into utilization management nursing may wonder how nurses in these positions improve the care of patients. While utilization management nurses do not provide direct patient care and see the patients whose lives they are affecting, they do have a tremendous impact on the quality and outcomes of patient care.
The main way that utilization management nurses help patients is by improving the overall healthcare delivery system. While this may not have the same glamour as resuscitating a patient or comforting a patient through a difficult procedure, it does make a significant difference in the lives of patients.
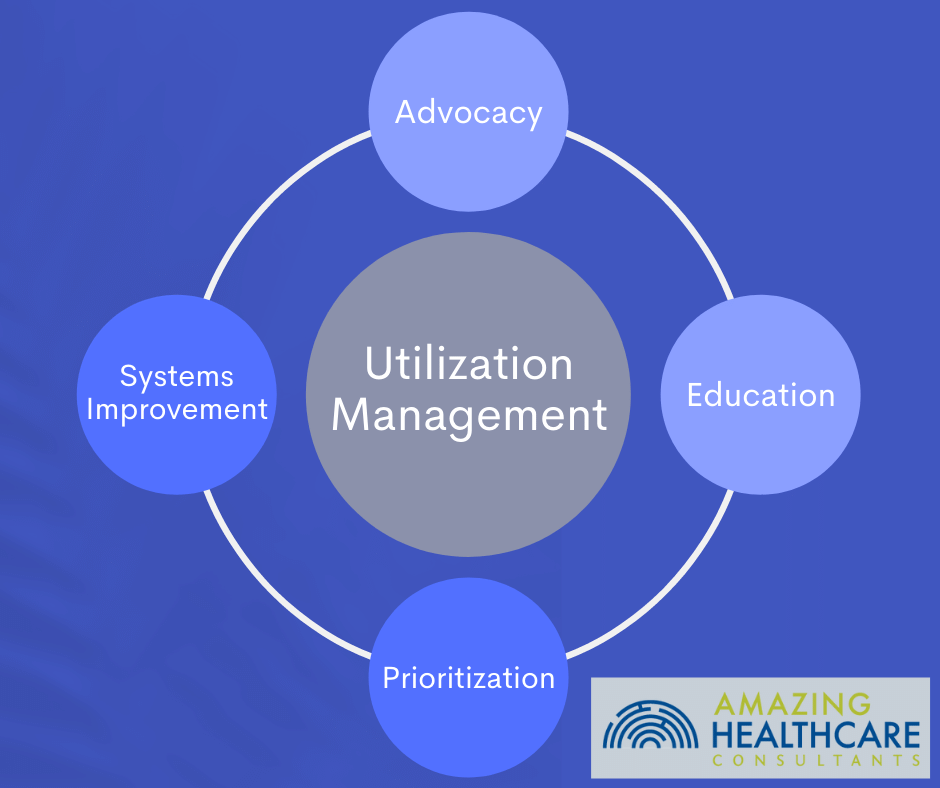
1. Advocacy
One of the most important roles of a nurse is to act as an advocate for their patients. This principle holds true for utilization management nurses, and nurses in this role will find that patient advocacy is a core part of the role.
One potentially difficult part of utilization management nursing is that this role involves advocating for the most good for the greatest number of patients possible instead of just advocating for a single patient at a time. Nurses, however, are very well equipped to understand how to advocate for groups of patients while considering the unique and separate needs that various patients in that group are likely to have.
2. Systems Improvement
Good nurses don’t just show up to work, provide patient care, then leave. They are actively engaged in improving the overall care delivery systems where they work. Nurses who are highly engaged in system improvement initiatives understand that the work they do in this area enables them to impact the care and outcomes of patients they will never see.
Utilization management nursing provides an ideal opportunity for nurses interested in improving care delivery systems, as this area of nursing is highly focused on making care efficient and affordable for patients.
By improving the overall care delivery system, utilization management nurses make a lasting difference in the lives of more patients than they could ever reach as a nurse providing direct clinical care.
3. Education
Providing education is a core part of any nurse’s job. While for many nurses this concept may conjure up an image of going over discharge paperwork or explaining medications to a patient, education can be focused on groups besides patients and their families.
Utilization management nurses provide education, but often targeted towards an audience that is more business and administrative oriented. Nurses in these roles will need to be able to explain nuances of clinical care in a way that is understandable, helping others to understand the importance of certain healthcare needs that may not be apparent to those without a clinical background.
4. Prioritization
Allocating limited resources as effectively as possible can, unfortunately, be perceived as taking from one group of patients to give to another. Nurses, however, do this all the time while providing patient care.
During clinical care, most nurses have multiple patient needs that they are having to address simultaneously. Nurses must determine which patient care activities require immediate attention and which can be delayed.
What Jobs are Available as a Utilization Management Nurse?
Utilization management nursing is its own specific field, and most jobs available in utilization management nursing are directly listed with this title.
Examples are utilization management nursing job titles are:
- UM nurse
- Utilization management nurse
- Utilization review nurse
- UM nurse consultant
- Utilization management nurse consultant
- Utilization management RN
- UM RN
- Utilization case manager nurse
While this list includes the most common job titles available for utilization management nurses, specific employers may have their own terms or titles for nurses in these positions.
The most common employer of utilization management nurses are healthcare insurance companies. These companies are primarily focused on resource utilization and rely on clinical experts, like utilization management nurses, to help guide their decision-making processes. Utilization management nurses may also play a role in helping to determine insurance policies and how the company will approach covering different types of clinical procedures.
Other employers of utilization management nurses include any healthcare facility that is large enough to invest in individuals who can assess and monitor how resources are used. This may include smaller hospitals, but will normally mainly include large healthcare systems that include multiple hospitals. These larger entities will be able to support larger teams that have a more administrative function, like utilization management staff. Larger entities are also more prone to waste, making the role of utilization management nurses more important in these organizations.
Job Outlook for Utilization Management Nurses
The job outlook for the nursing field in general is growing as the rate of attrition in the field is greater than the rate of new graduates. This is creating a greater number of vacant nursing positions in general, increasing the demand for nurses and the compensation being offered for nursing roles.
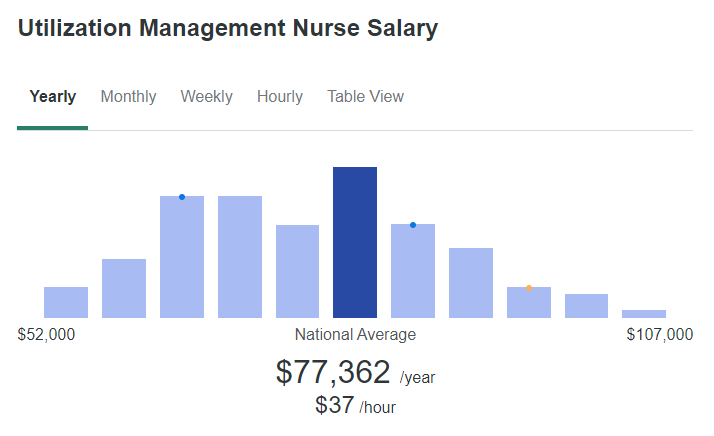
For utilization management nurses, specifically, the average national wage is over $77,000 per year. The demand for nurses in these positions is likely to grow as healthcare shifts to more centralized, larger entities primarily providing care.
The one factor that is unknown is how demand for non-clinical nursing positions changes. During the COVID-19 pandemic burnout for nurses has been a problem. This has seen many nurses shifting away from clinical nursing and towards other careers.
The shift away from clinical nursing may result in a greater supply of nurses seeking non-clinical nursing positions, such as utilization management nurse roles. The magnitude of this shift remains to be seen, along with how sustained such a shift would be.
What is Working as a Utilization Management Nurse Like?
Unlike many nursing roles, utilization management nurses can work completely from home, in many cases. While this does require more self-discipline, it also provides a degree of freedom that many nurses are not able to experience. Some work may require availability during normal business hours while other aspects of the work may be able to be completed on the nurse’s own schedule.
The amount of work will vary based on the employer and many other factors. Most utilization management nurses will work full-time positions, but will work during normal business hours. This allows for time off during holidays and weekends – another aspect of this position that is appealing to many nurses who may be accustomed to working unusual clinical schedules.
How to Become a Utilization Management Nurse
Most people who are considering working as a utilization management nurse are already nurses, however, being a nurse is the core, essential requirement for this role. Those who are not nurses will need to complete the education and licensing process necessary to become a registered nurse (RN).
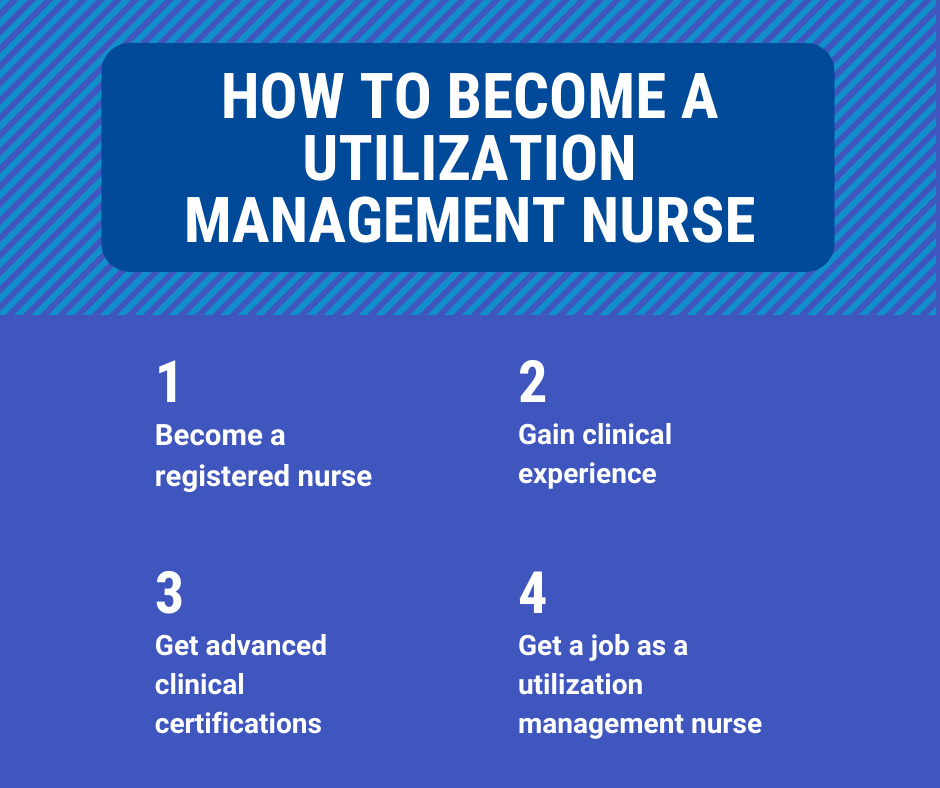
1. Become a Registered Nurse
Becoming a registered nurse requires an associate’s or a bachelor’s degree in nursing. While very rare, a diploma in nursing also allows eligibility to gain licensure as an RN. A bachelor’s degree is typically preferred and sometimes required for utilization management nurse roles. Upon completing a degree, licensure by the board of nursing in the state you are practicing in will also be necessary.
2. Gain Clinical Experience
While not strictly required to work as a utilization management nurse, it is highly improbable that a nurse without clinical experience would get a position in this role. Utilization management nurses add value because they understand the clinical process, and practical experience as a nurse will be a requirement in this role for almost any employer.
A nurse who ultimately wants to work as a utilization management nurse should have at least one year of clinical experience in a hospital environment before even considering making this career change. While one year is the bare minimum, at least three years of clinical experience in a hospital will probably be necessary in most situations.
3. Get Advanced Clinical Certifications
Nurses who wish to work as utilization management nurses are not required to get advanced clinical certifications, however, one or more of these certifications may help someone to get their first job in utilization management. The certification that is most relevant for aspiring utilization management nurses is the Certified Case Manager (CCM) certification.
4. Get a Job as a Utilization Management Nurse
Like many roles in nursing, getting an initial job and experience in utilization management nursing is ultimately the most important step in starting a career in this specialized area of nursing. With the correct clinical experience and clinical certifications, it should not be too difficult to get a position in utilization management nursing.
Utilization Management Nurses Make a Difference
While some nurses are drawn to utilization management nursing for the freedom of working from home or the ability to work normal hours that do not include holidays or weekends, nurses that stay in this field do so because of the difference they can make in the lives of many patients.
Nurses working in utilization management realize that they are making a difference in the lives of many more patients than they could ever care for in a clinical position, ultimately improving the long-term care of the patients they serve.
